It is almost like the air in a rural farming town is cleaner; it fills the nose with the scent of a freshly mowed hay pasture during the mid-September harvest season and we fondly recall the winding backroads leading us to a Friday night football game that seemingly shuts down the whole town. These feelings and memories pass from generation to generation even as the world around us grows more dependent on technology. Rural living is a national treasure deserving of being protected to ensure traditions continue, and that is why Spectrum Health Care expands its services to the residents of small towns in Missouri.
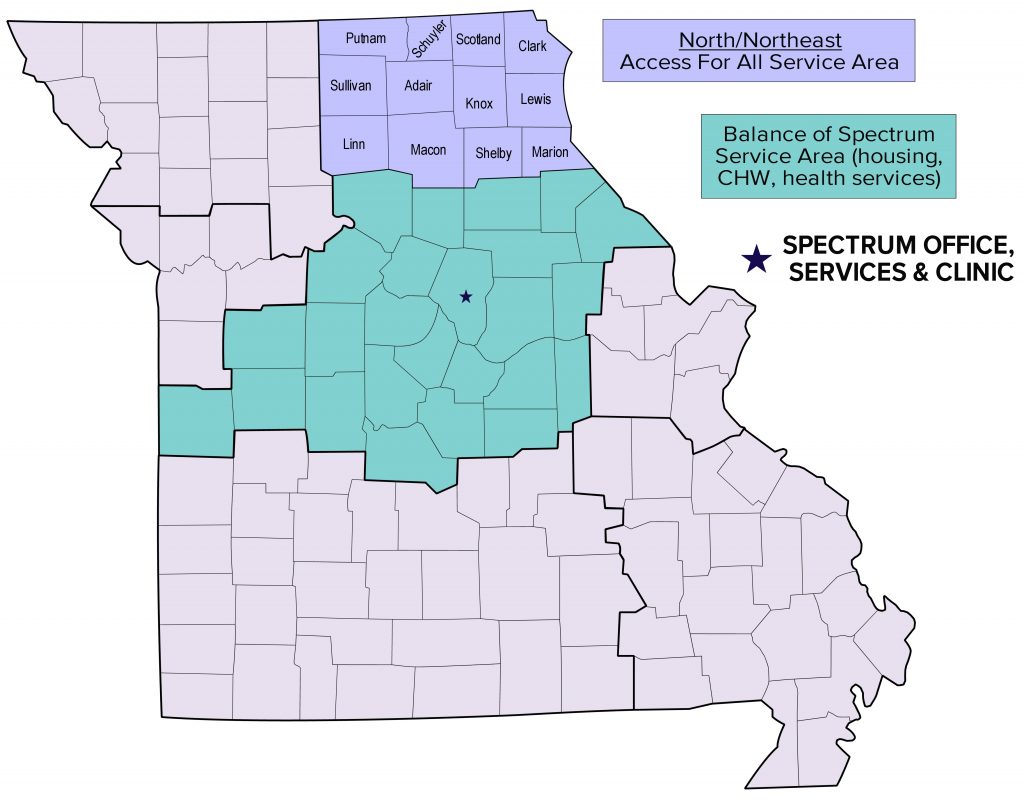 My name is Jessica Jones, and I am the North Missouri Community Health Worker, specifically serving the twelve rural counties located in the North/Northeast corner of the state: Adair, Clark, Knox, Lewis, Linn, Macon, Marion, Putnam, Schuyler, Scotland, Shelby, and Sullivan. Rural health has always been a passion of mine and I continue to support the counties I was born, raised, and live through my work with Spectrum Health Care. As we discuss the gaps in health care crippling rural areas, I hope to educate everyone as to the services and support Spectrum Health Care can provide to preserve the nostalgia of rural Missouri. (select map for larger view)
My name is Jessica Jones, and I am the North Missouri Community Health Worker, specifically serving the twelve rural counties located in the North/Northeast corner of the state: Adair, Clark, Knox, Lewis, Linn, Macon, Marion, Putnam, Schuyler, Scotland, Shelby, and Sullivan. Rural health has always been a passion of mine and I continue to support the counties I was born, raised, and live through my work with Spectrum Health Care. As we discuss the gaps in health care crippling rural areas, I hope to educate everyone as to the services and support Spectrum Health Care can provide to preserve the nostalgia of rural Missouri. (select map for larger view)
Tradition Leads to Grief and Discomfort
 I am the daughter of a 6th generation farmer, or as far as we can confidently track back. My hometown has a population of about 400 people, and houses a post office, the city hall, and a bar. My high school graduating class was 14 students; I knew each student in the school personally by name, often even being able to point out where they lived and name their parents and siblings. Over 90% of the high school student body was involved in Future Farmers of America (FFA), and our baseball diamond was parallel to a pasture of Black Angus cattle. I am a proud resident of rural Missouri, but rural Americans are suffering greatly from a lack of health care resources, and it is crippling farming traditions and communities.
I am the daughter of a 6th generation farmer, or as far as we can confidently track back. My hometown has a population of about 400 people, and houses a post office, the city hall, and a bar. My high school graduating class was 14 students; I knew each student in the school personally by name, often even being able to point out where they lived and name their parents and siblings. Over 90% of the high school student body was involved in Future Farmers of America (FFA), and our baseball diamond was parallel to a pasture of Black Angus cattle. I am a proud resident of rural Missouri, but rural Americans are suffering greatly from a lack of health care resources, and it is crippling farming traditions and communities.
I remember learning the FFA Creed in high school and reciting it religiously; there is a line in the second paragraph that constantly rings true in relation to rural areas and health care: “I believe that to live and work on a good farm, or to be engaged in other agricultural pursuits, is pleasant as well as challenging; for I know the joys and discomforts of agricultural life…” One of the biggest challenges and discomforts of agricultural life is the toll on the body: summers of bucking hundreds of square bales, being cornered between the 4-wheeler and one angry momma cow, riding in the tractor for twelve hours to put up the hay before the next day’s rainfall. In our younger years, our bodies would eventually bounce back from the previous day’s work, but years of continued stress on the body in this way can lead to chronic pain, arthritis, hypertension, heart disease, lung disease, hearing loss, and skin cancer. Untreated, these conditions can dramatically decrease the quality of life of farmers, as well as contribute to premature death.
Barriers to Proper Health Care
 Health professionals often refer to the term “social determinants of health” to explain differences in “the conditions in which people are born, grow, live, work, and age” and how these conditions are influenced by money, power, and access to resources. When we think of these conditions in rural areas, we fondly think of dirt and gravel roads, pastures of cattle, corn and soybean fields lining the roadways, and generations of families living just down the road. These characteristics of a rural area are nostalgic, but they come with consequences of limited area health services, populations with untreated chronic diseases, and lack of transportation.
Health professionals often refer to the term “social determinants of health” to explain differences in “the conditions in which people are born, grow, live, work, and age” and how these conditions are influenced by money, power, and access to resources. When we think of these conditions in rural areas, we fondly think of dirt and gravel roads, pastures of cattle, corn and soybean fields lining the roadways, and generations of families living just down the road. These characteristics of a rural area are nostalgic, but they come with consequences of limited area health services, populations with untreated chronic diseases, and lack of transportation.
 With the physical and mental toll farming can have, the next issue becomes the ease of access to health care services in rural areas. Ninety-seven of rural hospitals have closed since 2010 with little chance of being replaced with new care services, and remaining hospitals are unable to supply the high demand of care. Missouri hospitals are specifically in serious trouble, with more than 42% of Missouri hospitals vulnerable to closing their doors. Hospitals closing in rural areas will cause a gap in health care services, as many rural populations will have to travel farther to seek care or will refuse to seek care altogether due to the distance. In addition, a reduction in hospital services in rural areas will lead to a dramatic decrease in ambulatory and emergency services and an increase in preventable death due to delay in emergency care. Each second in an emergency can be the difference between life and death, leaving rural residents at a serious risk.
With the physical and mental toll farming can have, the next issue becomes the ease of access to health care services in rural areas. Ninety-seven of rural hospitals have closed since 2010 with little chance of being replaced with new care services, and remaining hospitals are unable to supply the high demand of care. Missouri hospitals are specifically in serious trouble, with more than 42% of Missouri hospitals vulnerable to closing their doors. Hospitals closing in rural areas will cause a gap in health care services, as many rural populations will have to travel farther to seek care or will refuse to seek care altogether due to the distance. In addition, a reduction in hospital services in rural areas will lead to a dramatic decrease in ambulatory and emergency services and an increase in preventable death due to delay in emergency care. Each second in an emergency can be the difference between life and death, leaving rural residents at a serious risk.
Consequences of Rural Health
 The closure of rural hospitals increases the importance of regular doctor visits to reduce the occurrence of major health events requiring emergency and hospital services. Again, rural areas fall short in the supply of qualifying health services within reach. In response, Centers for Medicare and Medicaid incentivized the creation of Rural Health Clinics (RHC) with a certification process and federal reimbursement of services to increase access of primary health services for rural residents. With the certification growing in popularity, Missouri and Texas house the most RHCs in the country, with more than 300 clinics statewide. Many RHCs offer no-fee or sliding-scale fees to reduce ability to pay or lack of health insurance from becoming a barrier to care. RHCs provide opportunities for primary health care services, such as monthly check-ups, physicals, and flu shot administration, but when it comes to specialized care for chronic diseases and surgical services, rural populations suffer as they struggle to find services within a reasonable distance and organize transportation.
The closure of rural hospitals increases the importance of regular doctor visits to reduce the occurrence of major health events requiring emergency and hospital services. Again, rural areas fall short in the supply of qualifying health services within reach. In response, Centers for Medicare and Medicaid incentivized the creation of Rural Health Clinics (RHC) with a certification process and federal reimbursement of services to increase access of primary health services for rural residents. With the certification growing in popularity, Missouri and Texas house the most RHCs in the country, with more than 300 clinics statewide. Many RHCs offer no-fee or sliding-scale fees to reduce ability to pay or lack of health insurance from becoming a barrier to care. RHCs provide opportunities for primary health care services, such as monthly check-ups, physicals, and flu shot administration, but when it comes to specialized care for chronic diseases and surgical services, rural populations suffer as they struggle to find services within a reasonable distance and organize transportation.
 Planning and organizing transportation to see a specialist is complicated for rural farmers. Farming is far from a predictable profession; someone would make millions if they could predict when farmers are going to have a frozen water tank, cattle running down the highway, or a hydraulic hose leak. If I had a dollar for every time plans changed last minute due to something happening on the farm, I could probably solve the student debt crisis across the country. This becomes a barrier to farmers seeking out specialty care. In addition, specialty care visits are more costly than a normal primary care visit. Without health insurance coverage, a specialist visit can cost hundreds, not including any additional lab testing and imaging the specialist requires. Combining the transportation and visit cost together adds up, leading to a cost barrier for farmers. Lack of proper chronic disease discovery and management contributes to the exacerbation of the disease and increases the risk of a major health event. The cost of specialty visits can be averted as many offices begin to offer 40-60% discounts for those without insurance coverage, or “self-pay.” However, this leaves transportation as a major barrier; rural areas often do not have existing public transit options available, and if transportation is available, routes and hours of operations are limited due to a lack of funding.
Planning and organizing transportation to see a specialist is complicated for rural farmers. Farming is far from a predictable profession; someone would make millions if they could predict when farmers are going to have a frozen water tank, cattle running down the highway, or a hydraulic hose leak. If I had a dollar for every time plans changed last minute due to something happening on the farm, I could probably solve the student debt crisis across the country. This becomes a barrier to farmers seeking out specialty care. In addition, specialty care visits are more costly than a normal primary care visit. Without health insurance coverage, a specialist visit can cost hundreds, not including any additional lab testing and imaging the specialist requires. Combining the transportation and visit cost together adds up, leading to a cost barrier for farmers. Lack of proper chronic disease discovery and management contributes to the exacerbation of the disease and increases the risk of a major health event. The cost of specialty visits can be averted as many offices begin to offer 40-60% discounts for those without insurance coverage, or “self-pay.” However, this leaves transportation as a major barrier; rural areas often do not have existing public transit options available, and if transportation is available, routes and hours of operations are limited due to a lack of funding.
Better Days on the Horizon
 As we have read in the last few years, the family tradition of farming is declining. Many farming journals cite climate change, political polarization, corporate farming, and globalization to be the main culprits, although I pose a different villain: healthcare, or the lack thereof. According to the National Rural Health Association, close to 20% of rural residents in America describe their health status as fair or poor. This is due to a combination of the social determinants of lack of access to health care services and transportation to address chronic health conditions such as heart disease, hypertension, diabetes, lung disease, and more. As our farmers’ health suffers, so does the occurrence of farming as a family tradition. Chronic health conditions can lead to medical debt swallowing the family farm whole, or even premature death. Let Spectrum Health Care help to make from these days forward the “better days through better ways, even as the better things we now enjoy have come to us from the struggles of former years.”
As we have read in the last few years, the family tradition of farming is declining. Many farming journals cite climate change, political polarization, corporate farming, and globalization to be the main culprits, although I pose a different villain: healthcare, or the lack thereof. According to the National Rural Health Association, close to 20% of rural residents in America describe their health status as fair or poor. This is due to a combination of the social determinants of lack of access to health care services and transportation to address chronic health conditions such as heart disease, hypertension, diabetes, lung disease, and more. As our farmers’ health suffers, so does the occurrence of farming as a family tradition. Chronic health conditions can lead to medical debt swallowing the family farm whole, or even premature death. Let Spectrum Health Care help to make from these days forward the “better days through better ways, even as the better things we now enjoy have come to us from the struggles of former years.”
 Here at Spectrum Health Care we provide support and services through our many health programs. Our Access for All Community Health Worker team is here to help you navigate the complex world of health, whether it be finding services, enrollment assistance in the ACA or Medicare, or cost assistance for primary health care services. If you or someone you know has a health care related question or need, give us a call at (573) 514-7312 or (800) 785-2437.
Here at Spectrum Health Care we provide support and services through our many health programs. Our Access for All Community Health Worker team is here to help you navigate the complex world of health, whether it be finding services, enrollment assistance in the ACA or Medicare, or cost assistance for primary health care services. If you or someone you know has a health care related question or need, give us a call at (573) 514-7312 or (800) 785-2437.

